Use the Immune System Student Learning Guide
It’s a dangerous world…
If you’re an organism, then the world can be a dangerous place.
If you’re an average sized human, then you’re about 70 kilograms of water, protein, nucleic acid, fat, and carbohydrate, organized into a unique pattern of dreams, desires, and aspirations. But to the parasitic worms, fungi, bacteria, and protists that we share the planet with, you’re a package of concentrated chemical energy, a moving mass of potential food and shelter. And a virus that could think would see your cells as protein-and-nucleic acid-making machines that hadn’t yet achieved their true destiny as virus factories. If that’s not enough, your dividing cells are just a few mutations away from going rogue, from breaking away from the team and becoming cancerous tumors, masses of cells that are of you, but not you. How does one survive in the face of these dangers?
You’re descended from a long line of survivors, each of which (going back right to the dawn of life) was able to fight off these pathogens (disease causing organisms) long enough to be able to produce offspring. In what follows, we’ll look at defenses shared by most organisms (barrier defenses, and non-specific responses), and then focus on the specific immune responses: a system that’s evolved exclusively among the vertebrates. Let’s go.
Page Outline
Use the outline below to jump to any section. You might find that if you haven’t watched my music video about the Non-Specific Immune Responses, doing so before reading further is a good idea. Note that it’s a great learning move to take the quizzes first, and then come back and read.
- Interactive Overview: Three layers of defense
- Defense Layer 1: Outer Barriers
- Defense Layer 2: Non Specific (Innate) Immunity
- Quiz: Non-Specific Immunity
- Interactive Lyrics
1. A Layered Defense System
We’ll start by defining what the immune system is. The immune system is “a network of cells, tissues, and organs that work together to defend the body against attacks by ‘foreign’ invaders.”vaccines.gov In vertebrates, this system has several layers, which you can meet by completing the diagram below.
[qwiz qrecord_id=”sciencemusicvideosMeister1961-Immune system, 3 Lines of Defense Concept Map”]
[q labels = “top”]
[l]Barriers
[fx] No, that’s not correct. Please try again.
[f*] Great!
[l]Fever
[fx] No. Please try again.
[f*] Great!
[l]infected
[fx] No. Please try again.
[f*] Good!
[l]Mucus
[fx] No, that’s not correct. Please try again.
[f*] Excellent!
[l]Non-Specific
[fx] No, that’s not correct. Please try again.
[f*] Excellent!
[l]Specific
[fx] No. Please try again.
[f*] Great!
[l]Three
[fx] No. Please try again.
[f*] Excellent!
[/qwiz]
We’ll explore these layers in the course of this tutorial and the next. But here’s a bird’s eye view.
- Your body’s first line of defense consists of barriers. In humans, that would include your (mostly) impenetrable skin, and your well defended mucous membranes (eyes, mouth, anus, vagina, etc.).
- If pathogens make it through these outer boundaries, they’re met by the non-specific, innate defenses. These consists of cells and molecules that attack a wide spectrum of pathogens. Non-specific defenses also include responses by tissues (such as the inflammatory response) and the entire organism (such as fever).
As mentioned above, some version of these two layers of defense are found among all multicellular eukaryotes. However, the last level is found exclusively in the vertebrate clade (the fish, amphibians, reptiles, birds, and mammals). And among us vertebrates, if our non-specific defenses don’t vanquish an attacking pathogen, then specific responses are brought into the fray.
In what’s below, we’ll explore the first two layers of our defense system. We’ll devote the entire next tutorial to the specific responses, which are found exclusively in our vertebrate clade.
2. Defense Layer 1: The Outer Barriers –Skin and Mucus Membranes
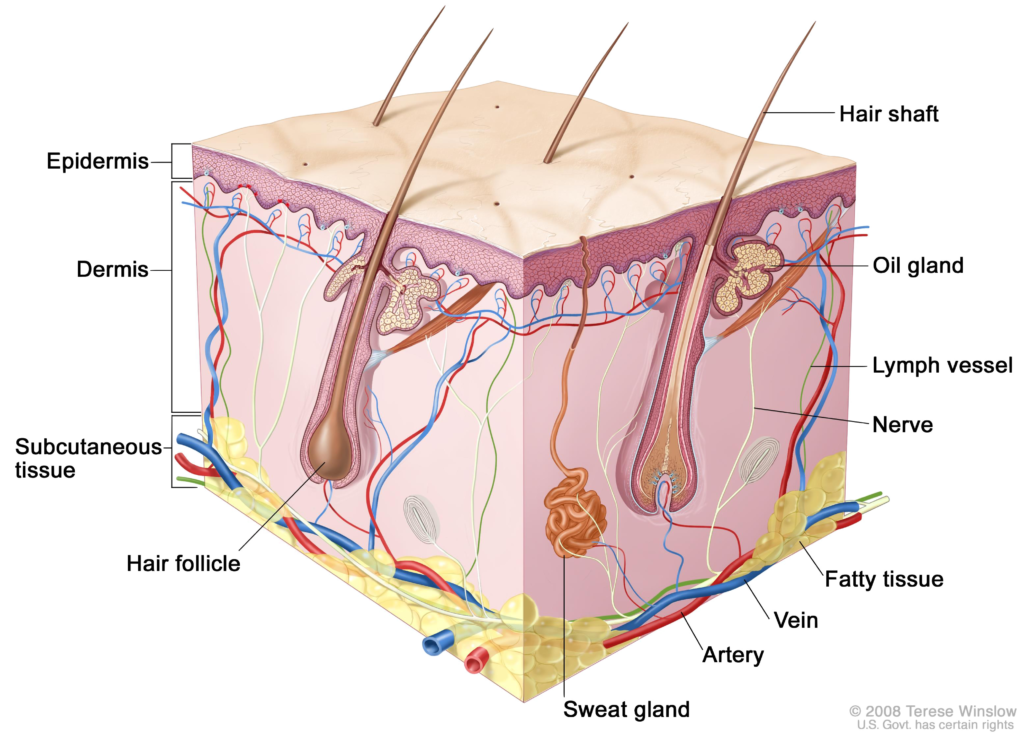
The skin is your outer boundary. For the most part, it’s impermeable to disease-causing organisms, collectively known as pathogens. That’s because the skin’s outermost layer, the epidermis, consists of tightly interconnected cells that are filled with a protein called keratin. This layer won’t allow water to pass through, much less bacteria or viruses.
While the epidermis might be impermeable, it’s far from sterile. Your skin is host to an entire community of bacteria, which is actually a good thing. These bacteria, your “resident flora,” outcompete any pathogenic microorganisms that might land on your skin. In fact, secretions from sweat and oil glands on your skin create an acidic environment that supports the growth of your resident bacteria, and inhibits microorganisms that might cause problems.source
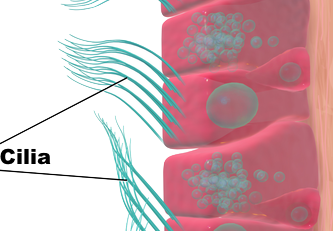
But while the skin serves as a protective barrier, you’re not a closed system. You need to take in food to provide yourself with matter and energy. You need to eliminate food that you can’t digest, along with metabolic wastes (like carbon dioxide and urea). All of these functions require orifices: openings to your body such as the mouth, nose, ears, eye sockets, urethra, anus, and vagina. To protect these orifices, you have mucous membranes. These membranes secrete mucus, a sticky protein that traps pathogens. Often, these membranes are lined with ciliated cells, that sweep pathogens towards the mouth or nostrils, where they can be expelled from the body (see the diagram to your right). Mucus also contains an enzyme called lysozyme, which attacks and breaks down the cell walls of a large group of bacteria. Lysozyme is also present in other mucous membrane secretions, including tears and saliva. Finally, note that anything that you swallow gets sent to the stomach, whose highly acidic secretions destroy most pathogens (but not all: there are animal and bacterial parasites that cover themselves with protective cysts that enable them to pass through the stomach and reach the less hostile intestines, where they can cause problems).
3. Defense Layer 2: Non-Specific (Innate) Immunity
Despite the effectiveness of our barrier defenses (skin and mucous membranes), pathogens can and do enter the body, entering through cuts in the skin or surviving mucous-membrane defenses. Once inside our bodies, these pathogens are met by the second layer of defense: the non-specific, or innate responses. Why are these non-specific? As we’ll see in the next tutorial, your immune system can unleash defenses that are targeted against specific invaders: for example, not just viruses in general, but against the measles virus; not just bacteria in general, but against tuberculosis. In contrast, the non-specific defenses can be unleashed against a variety of invading pathogens. And why are they innate? As we’ll see, the specific defenses involve development of immunological memory. As part of the specific responses, the immune system can remember the pathogens that have attacked it in the past, and, upon re-exposure to the same pathogen, fight it off more effectively than it did the first time. The non-specific responses that we’re about to explore involve no prior learning. That makes them innate: “determined by factors present in an individual from birth.merriam webster
3.a. Phagocytes
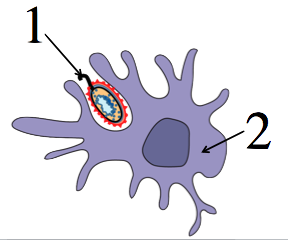
At the heart of the non-specific responses are phagocytic cells (phagocytes) that patrol the body, feeling around for pathogens. Phagocytes are a type of leukocyte, or white blood cell, that performs phagocytosis: they swallow and digest other cells. Below, you can see a cartoon version of phagocytosis, and a photograph of the process.
|
|
|
There are lots of phagocytic cells on patrol in various parts of your bodies. Here are two of the phagocytes you might read about in your text or other sources:
- Neutrophils: the most abundant type of white blood cell, and often the first phagocyte to arrive on the scene.
- Macrophages. The word means “big eater,” and you can find these cells throughout the body.
- Dendritic cells: these cells are on patrol in the skin and the linings of the nose, lungs, and gut.
Both macrophages and dendritic cells bring information about infections to the cells of the specific immune response (but we’ll learn about that in the next tutorial).
Note that in a typical AP Biology course, unless your instructor tells you otherwise, you don’t need to differentiate between these different types of cells. Just know that these phagocytes act as sentinels: “a soldier stationed as a guard to challenge all comers and prevent a surprise attack.”dictionary.com. When they meet these foreign invaders, our phagocytes respond by engulfing and digesting them.
But how do phagocytes know that the cells that they’re attacking are foreign invaders? Phagocytes have receptors for molecules typically associated with bacteria or other pathogens. One of these receptors is a Toll-like receptor, which “recognizes structurally conserved molecules derived from microbes” Wikipedia. If the phagocyte’s receptors bind with one of these microbial molecules, processes like chemotaxis (movement in response to a chemical signal) a will enable the phagocyte to follow a concentration gradient towards the microbe.
3.b. Natural Killer Cells
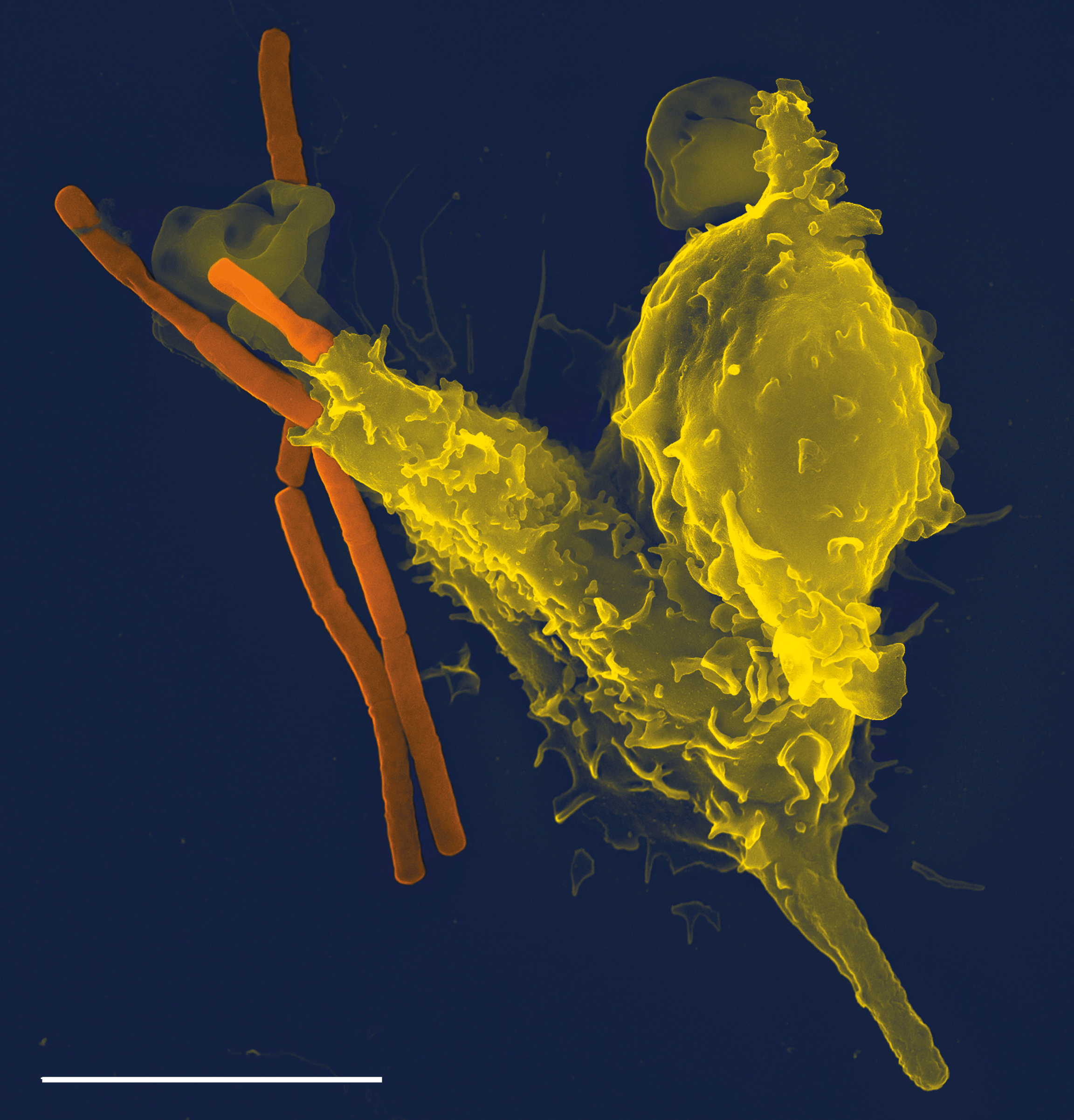
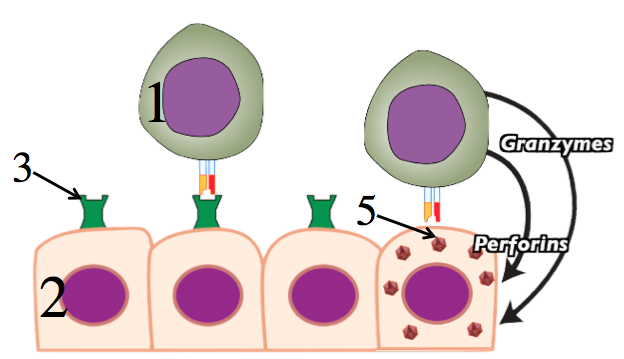 Another cellular response involves natural killer cells (shown at 1 in the diagram to your left). These cells’ primary role is to attack virus-infected cells, preventing these pirated cells from making more viruses. In this case, recognition is negative: rather than attacking based on the presence of a microbial molecule, the natural kill cell attacks when it senses the absence of a protein that’s on the surface of all body cells. This protein is called a Class I Major Histocompatibility (MHC) Protein, and it essentially acts as a flag that signals “I’m part of the team.” In the diagram at left, a class 1 MHC protein is shown at 3. When cells are infected by viruses (5) their ability to produce their normal complement of MHC proteins becomes compromised, and they’ll either have many fewer MHC proteins, or none at all. If this flag is missing, at it is in the last cell in the four tissue cells shown at left, the natural killer cell unleashes two weapons. Granzymes are molecules that induce the infected cell to commit apoptosis, or programmed cell death. Perforins open up holes in the infected cell’s membrane, killing the cells. Note that in addition to killing virus-infected cells, natural killer cells also target cells that have mutated to become pre-cancerous or cancerous (because these mutations can interfere with these cells’ ability to produce normal MHC proteins).
Another cellular response involves natural killer cells (shown at 1 in the diagram to your left). These cells’ primary role is to attack virus-infected cells, preventing these pirated cells from making more viruses. In this case, recognition is negative: rather than attacking based on the presence of a microbial molecule, the natural kill cell attacks when it senses the absence of a protein that’s on the surface of all body cells. This protein is called a Class I Major Histocompatibility (MHC) Protein, and it essentially acts as a flag that signals “I’m part of the team.” In the diagram at left, a class 1 MHC protein is shown at 3. When cells are infected by viruses (5) their ability to produce their normal complement of MHC proteins becomes compromised, and they’ll either have many fewer MHC proteins, or none at all. If this flag is missing, at it is in the last cell in the four tissue cells shown at left, the natural killer cell unleashes two weapons. Granzymes are molecules that induce the infected cell to commit apoptosis, or programmed cell death. Perforins open up holes in the infected cell’s membrane, killing the cells. Note that in addition to killing virus-infected cells, natural killer cells also target cells that have mutated to become pre-cancerous or cancerous (because these mutations can interfere with these cells’ ability to produce normal MHC proteins).
3.c.Interferons
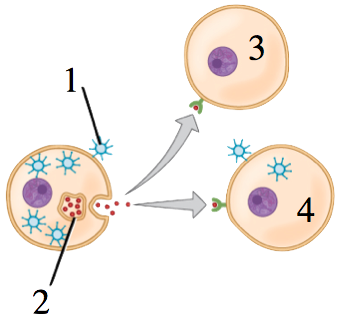
Interferons are another part of the non-specific response. Their function is easy to remember: interferons interfere with viral reproduction. Interferons (2, in the diagram to the right) are signalling proteins that are secreted by cells that have become infected by viruses (1). These signals are an infected cell’s way of saying: “I’m in trouble: you’ve got to save yourselves!” In uninfected cells (3), interferons have the effect of inducing production of enzymes that break down RNA and inhibit protein synthesis (both of which would have the effect of interfering with an infected cell’s ability to produce viruses). Interferons also induce apoptosis in cells that have become infected with viruses (4), which also short-circuits the viral reproduction cycle.
3.d.Complement
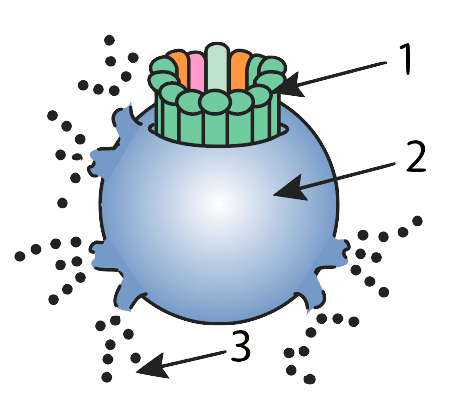 Complement consists of about 30 proteins that float freely in the plasma (the liquid portion of the blood). We’ll meet them again when we discuss specific immunity, but they also play a key role in the non-specific immune response. At the site of an infection, a cascade of enzyme-controlled reactions activates these proteins, which form a membrane attack complex (1). This complex creates holes in bacterial cell membranes (2), destroying these cells (“3” shows cytoplasm leaking out of the doomed pathogen).
Complement consists of about 30 proteins that float freely in the plasma (the liquid portion of the blood). We’ll meet them again when we discuss specific immunity, but they also play a key role in the non-specific immune response. At the site of an infection, a cascade of enzyme-controlled reactions activates these proteins, which form a membrane attack complex (1). This complex creates holes in bacterial cell membranes (2), destroying these cells (“3” shows cytoplasm leaking out of the doomed pathogen).
3.e. Inflammation
Inflammation is a tissue-level non-specific response that helps mobilize many of the cellular and molecular responses we’ve discussed above.

We’ve all seen inflammation. Here are some inflamed toes (probably caused by ballet-induced tissue damage, according to my students).
Inflammation can be caused by infection, too. Imagine that you’re working in the garden. You prick your finger on a thorn. Your skin, that impermeable barrier, is broken. Let’s see what happens next.
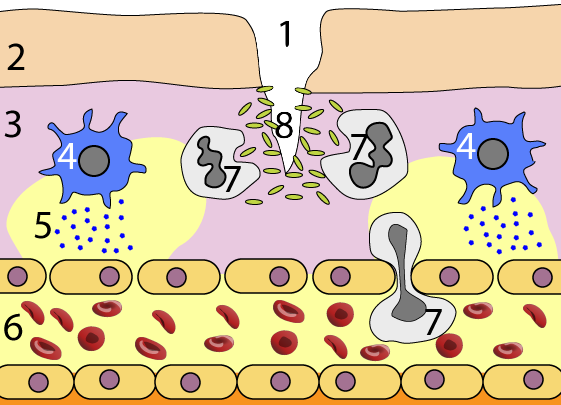
In the diagram to your left, “1” is the break in the epidermis (2). Bacteria (8) have entered the warm, moist dermis (3) and are multiplying.
In response, mast cells (4) release histamines (5). These signalling molecules bind with receptors on capillary walls, which loosen their hold on one another, becoming leaky (the entire capillary is indicated by “6”). This allows fluid in the blood to ooze into the tissue, causing the swelling associated with inflammation. The capillary walls become porous enough for phagocytes (7) to squeeze through, following a molecular trail that leads them to their bacterial prey.
Some of these phagocytic cells make the ultimate warrior move: they engorge themselves with bacteria until they die from ingested toxins…These dead white blood cells accumulate as pus: something to think about next time you see a pimple (itself a small inflammation of the skin). In addition, as we’ll see in the next tutorial, some of these white blood cells, particularly macrophages, can bring information about the infection to the cells that mobilize the specific immune response.
3.f. Fever
Here’s how I describe the effect of fever in part 1 of my Immune System Rap, which covers the non-specific responses.
A fever is a body-wide systemic inflammation,
The higher temperature inhibits germ replication,
And might also enhance immune cells’ phagocytic action
As fever ramps up our body’s chemical reactions.
While fever might be adaptive (possibly promoting phagocytosis and inhibiting germ replication), it is poorly understood. If you’re interested in the underlying mechanisms, click here to read about fever on Wikipedia. Otherwise, for AP biology, this is about all you have to know.
4. Non-Specific Responses: Checking Understanding
Before going on to the specific responses, let’s take a brief quiz.
[qwiz random = “true” use_dataset=”SMV_non-specific immunity” dataset_intro=”false” qrecord_id=”sciencemusicvideosMeister1961-Non-Specific Immune Responses, CFU”]
[h]Non-Specific Responses Quiz
[i]
[x][restart]
[/qwiz]
5.Immune System Interactive Lyrics
Another great way to learn the details of the immune system is by studying the rhyming lyrics to my Immune System 1: Non Specific (Innate) Responses song. Before or after watching the video, interact with the lyrics in the quiz below.
[qwiz use_dataset=”SMV_Immune System Interactive Lyrics Part 1 (non-specific)” dataset_intro=”false” qrecord_id=”sciencemusicvideosMeister1961-Immune System 1 (Non-Specific) Interactive Lyrics”]
[h]Immune System 1: Non-Specific (Innate) Responses, Interactive Lyrics
[i]
[/qwiz]